BRCA is the breast cancer gene found in everybody because it aims to repair the DNA, maintain other genes’ health, and help prevent cancerous gene changes. However, when the mutation damages any of these genes, the chances of cancer increase in the body.
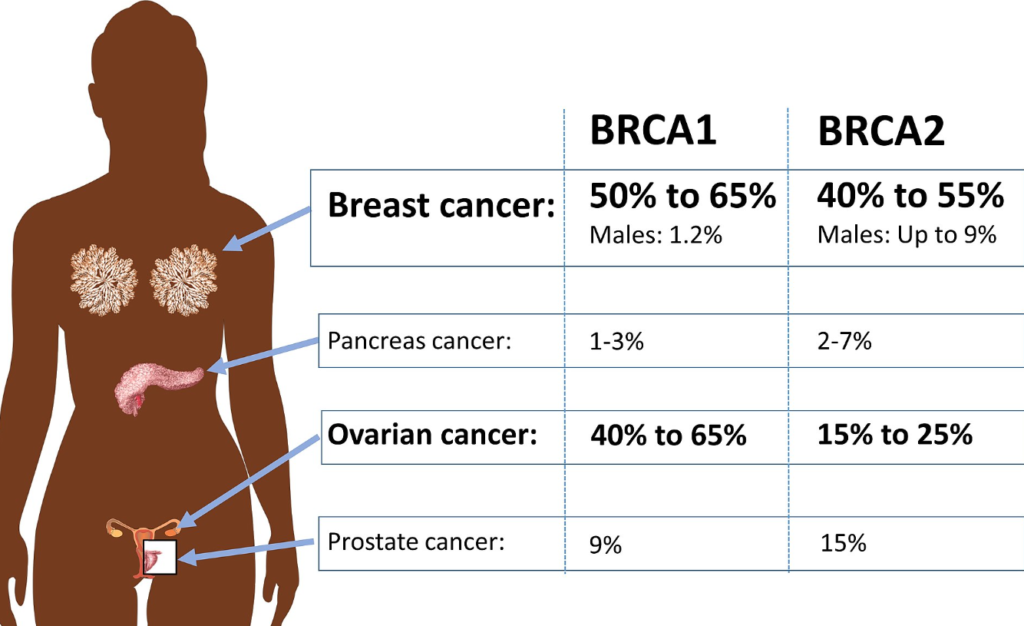
If you’ve inherited any of the damaged BRCA 1 and BRCA 2 genes, you risk developing breast or ovarian cancer in females and breast or prostate cancer in men.
Breast cancer is the second leading cause of cancer-related death in women. BRCA1 and BRCA2 are genes that play a role in repairing DNA. When these genes contain a mutation, they are unable to repair DNA effectively, which can lead to an increased risk of developing breast and ovarian cancer.
Research shows that certain people have a substantially higher risk of developing breast cancer than the average person. These people are known as high-risk individuals for this disease. High-risk individuals may benefit from having the BRCA gene test done before deciding on alternate treatments for breast or ovarian cancer.
If you have a strong family history of breast or ovarian cancer or if you’re Ashkenazi Jewish, your doctor may recommend getting tested for the BRCA1 and BRCA2 mutations as part of your routine preventive care. Testing for these mutations can be completed with a simple blood test.
Why take up BRCA gene testing:
BRCA gene testing determines if any mutations occur in your DNA. For example, mutations in BRCA 1 and BRCA 2 make you prone to:
- Breast Cancer
- Male breast cancer
- Ovarian cancer
- Prostate cancer
- Pancreatic cancer
- Melanoma
BRCA gene testing – Risk factors:
You must wonder who should get tested for the BRCA 1 and BRCA 2 mutation. There’s a chance you might be carrying either of the genes if you or your family member has:
- Been diagnosed with breast cancer before the age of 50.
- Previously had cancer in both breasts.
- A relative who has an experience with the BRCA mutation.
- Ovarian cancer, cancer in the fallopian tube, or primary cancer of the abdominal lining.
- An experience with triple-negative breast cancer.
- Faced breast cancer more than once.
- They suffered from both breast and ovarian cancer.
- History of experiencing breast cancer when young in two or more blood relatives like your parents, siblings, or children.
- Personal history of male breast cancer
- Personal history of ovarian cancer
- History of having two or more types of cancer.
It would be ideal for a family member with breast or ovarian cancer to get tested first. However, if they get tested and aren’t carriers of the mutation, it won’t be advantageous for other family members. Therefore, other genetic tests should be called upon, and a genetic counsellor can help you determine what tests should be considered based on your family and personal history.
Diagnosis of BRCA 1 and BRCA 2 mutation:
If your healthcare specialist uses newer methods of BRCA gene testing, i.e., saliva sample instead blood sample, it will be an easy process.
Previously, patients were advised to take an hour-and-a-half genetic counselling session before taking the blood sample. Now patients are given the option of spit testing. After the patient’s consent, a spit sample is handled via the ‘spit kit’ and shipped directly to labs.
Once the oncologists know whether or not the patient’s cancer is related to a specific gene, in this case, BRCA 1 or BRCA 2, it becomes simpler for them to move ahead with the therapy.
Understanding the gene mutation makes it easier for the physician to take steps regarding surgery or medical treatment.
Conclusion:
BRCA testing is a necessary step that people should take if they find out you’re related to someone who might have damaged BRCA 1 and BRCA 2 genes, as there is a chance you might have inherited it. If you test positive, you should work on getting proper treatment from your oncologist. Earliest management can help prevent the increased risk of breast and ovarian cancer.